In 1875, German scientists discovered a helical bacterium in human stomachs. In 1982, two Australian researchers, J. R. Warren (pathologist) and B. J. Marshall (gastroenterologist) rediscovered this bacterium among the microorganisms cultivated from human stomach samples. In 2005, they were awarded the Nobel Prize in Physiology and Medicine for having identified the role of this bacterium in gastritis and peptic ulcer.
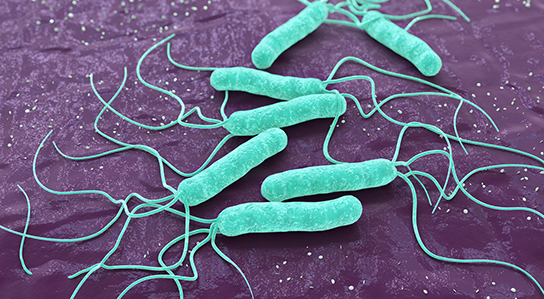
The bacteria
Helicobacter pylori is a Gram-negative bacillus, helical in shape, 3-5 µm by 0.3 µm, flagellated (2 – 6 polar flagella), non-spore forming, non-capsulated, and microaerophilic. Its reservoir is the human and primate stomachs, due to the acidic environment.
Epidemiology
- pylori infection is the second most common chronic bacterial infection in the world (after dental caries), infecting 45 to 50% of the world population. In France, the overall prevalence of H. pylori infection is between 15 and 30%: it is less than 5% in children but more than 50% in those over 60.
Helicobacter pylori: observed pathologies
Helicobacter pylori infection manifests itself in the form of acute gastritis, which often evolves into chronic gastritis. The penetration of the bacteria causes an inflammatory reaction of the gastric mucosa, with humoral and tissue immune reaction. In 85% of cases, the infection is asymptomatic; in 10 to 15% of cases, the gastritis will evolve into a peptic ulcer which may become complicated or recur (favoured by taking aspirin or NSAIDs), and in 1% of cases, into an adenocarcinoma or a MALT lymphoma. It should be noted that 70% of people with gastric ulcers and 90% of those with duodenal ulcers are infected with H. pylori.In children, ulcers are rare and less specific manifestations may be observed: abdominal pain, iron deficiency anaemia without a known cause, unexplained vitamin B12 deficiency, or chronic idiopathic thrombocytopenic purpura (ITP).
Search for Helicobacter pylori: Diagnostic indications
According to the HAS recommendations in 2019, the indications for H. pylori testing are as follows:
- Gastric or duodenal ulcer (history of ulcer or active ulcer, complicated or not);
- Before taking non-steroidal anti-inflammatory drugs (NSAIDs) or low-dose aspirin in case of a history of gastric or duodenal ulcer;
- Chronic dyspepsia with normal gastroscopy;
- Iron deficiency anaemia with no known cause or resistant to oral iron therapy;
- Vitamin B12 deficiency with no known cause;
- Risk factors for gastric cancer:
- Related to a patient who has had gastric cancer (parents, siblings, children);
- Patient with a predisposition syndrome for digestive cancers (HNPCC/Lynch);
- Patient with partial gastrectomy or endoscopic treatment of gastric cancer lesions
- Patient with gastric preneoplastic lesions (severe atrophy and/or intestinal metaplasia, dysplasia).
- Gastric Malt Lymphoma;
- Patient requiring bariatric surgery, isolating part of the stomach;
- Immunologic thrombocytopenic purpura in adults.
Helicabacter pylori: Diagnostic methods
Many tests are available. Among the direct diagnostic tests, some require an upper endoscopy allowing biopsies to be taken (culture, Polymerase Chain Reaction (PCR), histology), while others are non-invasive (carbon-13 urea breath test, search for H. pylori antigen in the stool); additionally, indirect serological tests are available.
Non-invasive tests
Carbon-13 urea breath test
This test, which can be used in children from the age of five years and in adults, does not require any special conditions for storing samples. It is the best diagnostic and control technique for H. pylori eradication when an endoscopy is not necessary. However, the procedure is sometimes complex and false negatives may occur after antibiotic therapy or use of antisecretory drugs such as proton pump inhibitors (PPIs). Pre-analytical precautions The subject must have been fasting since the previous day, be at rest, and must not eat, drink or smoke during the test. The subject must have stopped all antibiotic treatment at least four weeks before the test and all anti-secretory treatment (PPI, anti-H2) at least two weeks before the test, as well as any antacids and gastrointestinal dressings (Maalox®, Rennie®, Smecta® …) for at least 24 hours. The reliability of the tests is excellent, with a sensitivity of 93.3%, specificity of 98.1%, PPV of 97.7% and an NPV of 94.6%. PrincipleThe breath test uses carbon isotopes (12C in the majority; 13C in small quantities in nature, stable). A 13C-labeled urea solution is drunk by the patient. In the presence of H. pylori urease, the 13C-labeled urea is degraded in the exhaled air; in the absence of urease, it is absorbed and metabolised.The test consists of measurements of 13C-labeled CO2 in exhaled air. Precautions should be taken when collecting the exhaled air:
- Identify the two T0 tubes and the two T30 tubes
- Uncork the tube
- The free end of the straw at the bottom of the tube
- Patient takes a regular breath, blows gently and continuously for at least 15 seconds
- Appearance of mist at the bottom of the tube (no saliva)
- The tube is removed by sliding it along the straw, keeping it vertical
- As soon as the straw is removed, the tube is quickly recapped
- Replace the four tubes in the kit box
Tests for Helicobacter pylori antigen in stool
The available tests have satisfactory performance, particularly in terms of specificity (≥ 98.9%); however, they require refrigerated or frozen stool if the preanalytical delay is too long, and false negatives are also found in patients on PPIs. Comparing the sensitivity and specificity of H. pylori Ag detection in stool with the respiratory test shows similar performance with a slight advantage for the respiratory test.
Serological Tests
Infection occurs most often in childhood. IgG appears in 2 to 3 weeks and its concentration remains high as long as the infection persists. IgM is too transient to be detected. Serological tests are interesting diagnostic tests because IgG is easily detected by ELISA or chemiluminescence techniques. The negative predictive value of the available tests is excellent; they only require a blood sample and are inexpensive and reimbursed. The assay can be delayed if the serum is frozen. Furthermore, serology is the only method that is not affected by changes in the stomach. Indeed, the bacterial mass may decrease below the detection limit of other methods, transiently in the case of antibiotic or anti-secretory treatment, or permanently in the case of pre-neoplastic or neoplastic lesions. However, serology results may be close to the threshold value if the immune response is weak, and positive serology is not evidence of active infection. Serology cannot be used for treatment follow-up because the decrease in antibody concentration is slow, usually 4 to 6 months, and IgG may persist for months or even years after eradication. It is especially interesting if it is impossible to stop PPIs before the diagnostic test. If it is negative, the diagnosis can be ruled out; if it is positive, a gastroscopy is recommended with biopsies for anatomopathological and bacteriological examinations.
Invasive tests
Histology on biopsies
Histological examination is performed on at least two antral biopsies and two fundic biopsies, taken under endoscopy. Its sensitivity is excellent if the anatomopathologist is experienced. This examination allows the detection of H. pylori, but also the estimation of the severity of the lesions.
Culture
The biopsies are cultured as soon as they are taken: they can be kept refrigerated for a maximum of 24 to 48 hours in Portagerm® Pylori medium, or frozen at -20°C. Upon arrival at the laboratory, grinding of the biopsies is a key element of the diagnosis. Culture is performed on agar media that are less specific for H. pylori. The growth of H. pylori is difficult (reading every 48 hours), in the form of small translucent, non-pigmented, non-hemolytic colonies, 1 mm in diameter. Incubation is continued for up to 14 days in a microaerophilic atmosphere. The specificity of this examination is excellent and its sensitivity good in experienced laboratories (this depends mainly on the pre-analytical conservation); however, 10% of false negatives compared to PCR should be noted at the National Reference Center for Campylobacters and Helicobacters (CNRCH). The main advantage of culture is that it allows an antibiogram to be performed. Given the evolution of H. pylori strain resistance in France, antibiotic susceptibility testing is recommended, especially in cases of failure to eradicate prior to first-line treatment.
Polymerase Chain Reaction (PCR)
PCR can be performed on gastric biopsies. The performance of PCR kits marketed in France has been evaluated by the CNRCH and is excellent. The main advantages of PCR are its very good performance, especially in terms of sensitivity compared to culture, the fact that the pre-analytical conditions are less strict than for culture, the rapid delivery of results and, above all, the possibility of searching for mutations associated with resistance to clarithromycin and, possibly, levofloxacin, or even to other antibiotics useful for the treatment of H. pylori infections.